In developing countries barefoot midwives are armed with karuna and moxie and in many instances, little else.
The life of a Barefoot Midwife is anything but easy. Barefoot Doctoring has ancient roots for it has been around since the first person attempted to help another. Indeed any attempt to relieve another’s pain and suffering is a form of Barefoot Doctoring. Compassion, wisdom and skill are the necessary certificates, and consent is the only license needed to engage in the art of healing.
Many Barefoot Doctors are Herbalists, Midwives, Ayurveda Practitioners, Apothecarians, Bush Doctors and even Shamans. The more holistic and natural approach in combining many types of healing, the better because Barefoot Doctors must make due with what they have. Some practitioners receive word of mouth training and some are self-taught. What defines a Barefoot Doctor is their intention to move the life in question forward toward a higher quality of existence. A noble and tough task for these unsung heroes.
Technology has facilitated many of today’s medical advancements and breakthroughs. So how is this knowledge and technical know how trickling down to benefit the world’s Barefoot Midwives? Trickling slowly but gathering steam with the help of groups like Maternova, Mobile MAMA Alliance and Save the Mothers. Maternova aims to cut through red tape and get desperately needed low tech solutions and midwife kits to the ones who need it the most. MAMA is a mobile phone health initiative partnership led by USAID, Johnson & Johnson and India’s ARMMAN that sends life saving text message alerts to expecting mothers. Save the Mothers equips professionals in developing countries with the know how they need to improve the health of mothers and babies.
Problematic pregnancies due to preeclampsia have been around for a very long time and documented cases date back 2000 years. Did you know that Eclampsia is a Greek word that means a person’s lights are turned off? According to the Columbia University Mailman School of Public Health preeclampsia is on the rise. For this study doctors examined data on 120 million births between 1980 and 2010 from national hospital discharge surveys. This is the largest study conducted to date to analyze changes in rates of preeclampsia in the US. In 2011 the WHO indicated the incidence of preeclampsia to be 7 times higher in developing countries than in developed countries. A by-product of the poor trying to make ends meet by eating cheap food that is high in starch and salt.
So what can you do to help prevent 800 women from dying every day in childbirth? If you are as shocked as I am about this staggering number, then perhaps you might want to consider becoming a midwife. Today it is easier than ever with the plethora of quality online courses offered at venues like Missouri’s Maryville University
Furthermore, how can we as a community of caring individuals better equip Barefoot Midwives with life saving knowledge and low tech solutions? Simple: By sharing the following data with as many midwives as we can reach through the Internet and Social Media.
1. Prevention is key so midwives should instruct expecting mothers to start with a balanced pregnancy diet. Fresh, healthy, wholesome foods and to stay away from junk food, fried foods and sodas. Consume multiple small portions throughout the day of fresh meals. Pregnancy diets should include fermented milk and yoghurt, whey, eggs, pumpkin seeds, sesame seeds, peanuts, chick peas, tofu, moringa, kale, spinach, lentils, leafy lettuce, dandelion greens, broccoli, okra, collards, cauliflower, cabbage, beets, raw asparagus, tumeric, avocado, potatoe skins, watermelon and bananas. A new study has shown vitamin D, calcium, magnesium and sulfur deficiency to be a risk factor in developing preeclampsia so pregnant women really should try to eat the range of foods mentioned above including foods high in sulfur. Drink plenty of purified water (SODIS), coconut water, tumeric tea, white mulberry tea, red hibiscus tea, dandelion tea, raw beet juice, orange juice and aloe juice. Nota Bene: A probiotics in pregnancy analysis conducted by the Norwegian Institute of Public Health determined that probiotic milk intake in late pregnancy was significantly associated with lower preeclampsia risk (adjusted OR: 0.80 (95% CI 0.68 to 0.94) p-value: 0.007). Probiotic intake during early (but not before or during late pregnancy) was significantly associated with lower risk of preterm delivery (adjusted OR: 0.79 (0.64 to 0.97) p-value: 0.03).
Pregnant women should soak in Epsom salts a couple of times a week. In absence of a tub, consider applying Epsom salts dissolved in warm water in a bucket and have pregnant mother’s soak their feet or dip a rag and apply externally. The recommended dose is 1 cup of Epsom salts dissolved in 1 quart of warm water but always go with the recommended dosage listed on the package. Soaking in Epsom salts helps to reduce ankle swelling and is a safe easy way to increase sulfate and magnesium levels in a pregnant mother’s body. Midwives should apply Epsom Salts Oil to the skin because it gets absorbed quicker into the blood stream of an expecting mother. Nota Bene: The above noted description is a low tech application of Epsom salts for treating Preeclampsia. The high tech treatment for severe cases of Eclampsia is to inject an Epsom salt solution intravenous which MUST be administered by a doctor and ONLY in a hospital setting.
2. Another important step in prevention is early detection. If a patient shows any signs of having preeclampsia, the midwife should try to get her patient to a clinic ASAP for more thorough analyses. Preeclampsia in new mothers may often go disregarded since they may not know what they “should” be feeling. Therefore family members and midwives are key partners in preventing maternal deaths by intervening and getting medical attention when their spouse or partner complains of shortness of breath, relentless headache, drowsiness, difficulty speaking, blurred vision, seeing spots, nausea and vomiting. One of the easiest ways to determine if a pregnant mother may have preeclampsia is to see if she has protein in her urine. The low tech diagnostic for protein in urine is simple. Get a urine sample from the patient, preferably right after she gets up in the morning or 2 hours after a meal. Place the urine in 2 separate glass jars and place one in hot water for a few minutes. Remove the jar from the hot water and compare it to the non heated urine. If the heated urine sample is cloudy, then it contains protein which is an indicator she has preeclampsia. Next test for high blood pressure signs which develop in women after 20 weeks gestation. In absence of a blood pressure meter the midwife will need to take blood pressure the old fashioned way and regularly. First make sure the pregnant mother has not had any coffee or has been exposed to cigarette smoking and is sitting down in a relaxed position. Then hold the mother’s arm so it is straight with the underside facing upwards. Feel around their wrist, using your index and middle finger of one hand until you find the pulse (do not use your thumb). Use a clock with a second hand and carefully count how many beats you feel in a full minute. A normal resting heart rate for an adult is 60 to 100 beats a minute. To test the baby’s heartbeat midwives can use a home made Doppler (see video for DIY instructions) and fetal heart string beads (purchase from Maternova) or try to make the heart strings beads if necessary (bead sequence is 29 white beads followed by 10 green and 11 red). The midwife will need to assess the position of the baby and place the Doppler on the mother’s belly to hear the baby’s heartbeat. Hold the Heart String Beads with the red beads facing the body and brace the 1st white bead between your thumb and forefinger. You will need to use a 15 second timer or have someone count down 15 seconds. Start pressing a bead each time you hear the baby’s heartbeat. After 15 seconds you will need to look at where you have landed on the bracelet. If you are in the white section, the heartbeat is too low. Provide the patient with a small amount of sage tea to help raise her blood pressure. Also ask the patient if she has not eaten and if so, provide nourishment (preferably a banana which has potassium and is good for a weak stomach). If she can’t hold her food down, then provide some ginger tea. If she can’t hold the tea down then place a rag that has been dipped in ginger tea on the mother’s belly button so it can get absorbed into her system. Ginger is the best tool for treating nausea. Retest the heartbeat of the mother and baby. If the midwife landed on the Green bead, the heartbeat is normal. The Red, the heartbeat is too high. If the heartbeat of the mother and baby is too high give the mother some tumeric tea or baobab fruit tea to drink or clean water and retest their heart rate. If their heartbeat remains elevated then the midwife should take her patient to the nearest hospital or clinic. Remember: eclampsia warning signs include confusion, headache, drowsiness, difficulty speaking, blurred vision, seeing spots, nausea and vomiting. If present get your patient to the nearest hospital right away. If a hospital or clinic is too far away and a pregnant mother starts having seizures, turn her on her side so she won’t swallow her tongue and rub Epsom Salt Oil on the mother’s forehead and her belly button so it will get absorbed into her system quicker. If the pregnant mother is conscious ask her to cough really hard multiple times (cough CPR) and put a pinch of cayenne pepper in her mouth (promotes blood circulation). If she is unconscious and is not breathing, administer CPR until she stabilizes. To administer CPR roll the patient on her back and start chest compressions. Place the heel of your hand on the center of her chest. Put your other hand on top of the fist with your fingers interlaced. Press down so you compress the chest at least 2 inches in adults and children and 1.5 inches (equivalent to 2 fingers) in infants. One hundred times a minute or even a little faster is optimal. Now open the airway with a head tilt and chin lift, pinch closed the nose of the patient. Take a normal breath, cover the patient’s mouth with a homemade CPR mouthpiece (retrofitted plastic soda bottle with gauze soaked in aloe vera) to create an airtight seal, and then give 2, 1-second breaths as you watch for the chest to rise. Continue compressions and breaths – 30 compressions, two breaths – until the patient responds.
3. Many believe that “delivery is the cure” for preeclampsia but today it is known that in many cases the after effect of preeclampsia continues for 2 weeks following delivery and sometimes up to 6 weeks postpartum. Therefore midwives and spouses will need to remain mindful during this period. The new mother must maintain her healthy diet and should breastfeed her new born baby. Remember if the mother is malnourished then so will the baby. An improper diet is the main culprit behind maternal mortality in developing countries. It is the main cause of seizures and hemorrhaging. A tea made from the leaves of the stinging nettle plant is beneficial during pregnancy labor due to its rich mineral value and vitamin K, which guards against excessive bleeding. If the midwife does not have stinging nettle then she can give the Mother some dried ground up basil leaves mixed with peanut butter when contractions start. Dried basil has a higher percentage of vitamin K versus fresh basil leaves. Vitamin K is also a good supplement to strengthen the fetus. A uterine massage is also key for preventing postpartum hemorrhage. Breastfeeding is extremely important for the health of the baby. A mother’s milk right after giving birth is known as “liquid gold” or colostrum. In many countries colostrum is discarded because it is thick and yellow. This milk is very rich in nutrients and antibodies that protect the new born baby.
4. Hygiene is crucial so midwives need to keep soap handy and in absence of soap keep some home made soap in a vial in their midwife kit or even a piece of aloe vera. Soap can be made by soaking soap seeds in water and/or soaking peeled yucca root in water to release the saponins. The younger the yucca root, the more it will foam and lather. In absence of water you can peel aloe vera and use the gel to sanitize your hands, treat wounds including a new born’s umbilical cord. Aloe contains 6 antiseptic agents that kill bacteria, viruses and fungus and can be taken internally or applied externally. Regarding cutting the new born baby’s umbilical cord, it is now known that the umbilical cord contains Wharton’s Jelly and this protects the arteries and veins in the cord. This is why knots and tangled babies are fine the majority of the time because Wharton’s Jelly keeps the cord firm and unable to collapse. After the birth the jelly slowly “clamps” down on the arteries first, then the umbilical vein. Usually after 3 minutes the cord will slowly turn from heavy and firm (and colored) to limp and white. At this point it can be cut with little to no mess at all – no medical clamps needed! The 30 seconds rule for cutting umbilical cords no longer applies. Interestingly enough umbilical cord care research has also demonstrated that using the mother’s milk to treat the umbilical cord twice a day helps the cord detach sooner and prevents infection. Lastly the yellow creamy vernix that is coated on the new born’s skin keeps the baby warm and is also an antibacterial that protects the baby so just like the cord, don’t be too quick to cut and don’t be too quick to bath the new born baby.
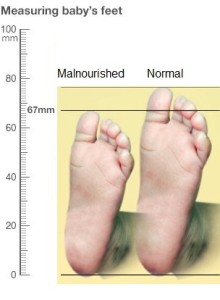
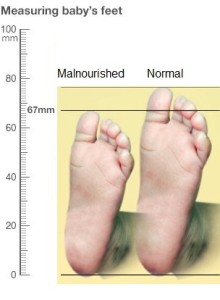
5. New born assessment and care. The midwife should wipe and dry the new born baby using clean, warm towels. Swaddling should not be done too tight and should be loose around the hip and leg areas. If swaddling is done incorrectly it can lead to hip problems. Midwives can use the following chart to gauge the baby’s foot size and determine if the new born is under weight and size for a normal baby. If the baby appears to be malnourished then most likely the mother is too. In this case the best treatment for the malnourished mother is a paste made from cooked black chick peas or regular chick peas if you do not have the black variety. In absence of this a home made peanut butter paste will suffice as this is the main ingredient in Plumpy Nut.
It is important to mention that currently the intravenous use of magnesium sulfate in severe preeclampsia and eclampsia in a hospital setting is supported by The American Congress of Obstetricians and Gynecologists (ACOG), World Health Organization (WHO), Society of Obstetricians and Gynaecologists of Canada (SOGC), and the National Institute for Health and Clinical Excellence (NICE).
It is also noteworthy that the SOGC and WHO both have provided statements that support the use of soaking in magnesium sulfate in low tech settings for the treatment of preeclampsia.
Please do your part and help us spread this life saving information with your #midwife connections and counterparts so we can put an end to #maternalmortality. Because #everymothercounts!